UTCSP Translational Seminar Series | CPIN Distinguished Lecture Presents: Dr. Bushnell
You can view the talk here:
Beyond Opioids: Engaging Endogenous Pain Modulation in the Brain
Dr. M. Catherine Bushnell, PhD, is President of IASP, as well as Scientist Emerita at the National Center for Complementary and Integrative Health (NCCIH) at the US National Institutes of Health (NIH) and the Harold Griffith Professor Emerita in Anesthesia at McGill University. She holds a Ph.D. in Experimental Psychology from the American University and received postdoctoral training in neurophysiology at the NIH. She was Founding Director of the McGill University Alan Edwards Centre for Research on Pain (2003-2009) and Director of the NCCIH Intramural Research program (2012-2020). She has received Lifetime Research Achievement Awards from the Canadian Pain Society and the American Pain Society. Her research interests include forebrain mechanisms of pain processing, psychological modulation of pain, and neural alterations in chronic pain patients.
Nonionotropic NMDA receptor activity enables reversal of pathological pain in mice
Current treatments for chronic pain tend to conceal and dampen nociceptive processing rather than target its root causes.
Written by:
Quinn Pauli
Edited by:
Georgia Hadjis
Current treatments for chronic pain tend to conceal and dampen nociceptive processing rather than target its root causes. Many forms of chronic pain are thought to involve sensitization of spinal pain networks. Sensitization of nociceptive pathways shares several mechanisms with the strengthening of neuronal pathways in the brain which gives rise to memory. Like memory traces in the brain, it has previously been shown that sensitized nociceptive pathways can be destabilized and modified upon reactivation. However, the cellular mechanisms underlying the destabilization of ‘pain memory traces’ in the spinal cord are poorly understood. UTCSP member Dr. Rob Bonin and his colleagues performed a battery of behavioural, molecular, and electrophysiological experiments in mice to study the cellular mechanisms involved in the reversal of pain hypersensitivity.
To selectively reverse mechanical hypersensitivity in commonly used mouse models of pain, the authors of this study leveraged parallels between pain and memory by focusing on a nonionotropic form of NMDA receptor-mediated signaling involved in the weakening of synaptic connections in the brain. They found that reactivating sensitized sensory pathways, while pharmacologically inducing nonionotropic NMDA receptor activity, reverses mechanical hypersensitivity. Similarly, potentiated spinal cord pathways can be reactivated and weakened ex vivo by nonionotropic NMDA receptor activity. The authors identified specific synaptic proteins that are degraded to reduce mechanical hypersensitivity upon reactivation, many of which are also degraded during memory modification.
The results of this study published in Science Advances reveal a unique signaling pathway which enables reversal of pathological pain in mice by targeting its underlying cellular causes. Ultimately, gaining a better understanding of the dynamic regulation of pathological pain could lead to new therapeutic options for treating chronic pain conditions in humans.
The results of this study published in Science Advances reveal a unique signaling pathway which enables reversal of pathological pain in mice by targeting its underlying cellular causes.
UTCSP Translational Series
We are excited to announce our upcoming Translational Seminar Series, in partnership with CPIN, IASP, and CPS
Join us on August 31st at 12pm to connect with your fellow community members and dive into a talk by Dr. Catherine Bushnell on Beyond Opioids: engaging endogenous pain modulation in the brain.
When:
Aug 31, 2023
12:00pm-2:00pm
Lunch: 12pm -1pm, Talk: 1pm - 2pm
Where:
Hart House Debates room
Virtual via zoom (1pm-2pm)
Register by:
Aug 31
Virtual via zoom registration:
Trainee Welcome Event
Thank you to everyone who came out to our trainee welcome event, and made it a great success!
Seed Grant
We are pleased to announce the UTCSP SEED GRANT opportunity!
This opportunity will provide funding for 1 year, with up to $30,000. Principal applicants must be UTCSP members with a faculty appointment to the University of Toronto who are able to hold research funds at the University of Toronto.
Priority areas include:
- Projects that address the opioid crisis.
- Interdisciplinary/cross faculty collaborative pain research.
- Pain education research.
Full information to apply: here.
Application form: here.
How to apply: Please send the application package (all documents in one PDF) to utcsp@utoronto.ca.
Deadline:
Oct 13 2023
Grant amount:
$30,000
History of the UTCSP
“The UTCSP has provided me with an unparalleled network of scientific and collegial support. It has broadened the scope and potential of my pain research to change clinical practice. In addition, the centre has provided my doctoral trainees with unique development opportunities. Taken together, the UTCSP has strengthened my ability to be a productive scientist and therefore contributed significantly to my tenure appointment.” -Dr. Craig Dale
History
The establishment of the UTCSP in 1999 was novel for that time since no such centre existed elsewhere in the world. It was also somewhat fortuitous in that the University of Toronto administration decided at this time that its different faculties and programmes needed better integration in their educational and scholarly programmes. With that in mind, it developed in the late 1990s a request to faculties for applications to establish a pioneering UofT-funded academic programme that would bring together staff and students in different faculties to engage in interfaculty/interdisciplinary educational and scholarly activities.
Also fortuitous was that the Council of Health Sciences Deans was chaired at that time by Barry Sessle, the Dean of the Faculty of Dentistry who happened to be a pain researcher and President of The International Association for the Study of Pain. It also happened at that time that there was a cadre of pain clinicians, researchers, educators and trainees spread around the different UofT health science faculties and their affiliated hospitals, but there was limited collaboration and coordination of their educational and scholarly activities. Dr Sessle and several others in the UofT pain community (e.g. Drs. Jonathan Dostrovsky, Allan Gordon, David Mock, Michael Salter, Bonnie Stevens, Judy watt-Watson) realised that pain was an ideal topic for such an interdisciplinary focus as envisaged by the UofT administration and an opportunity to bring together the diverse group of pain clinicians, researcher and educators and trainees in a Centre fostering collaboration and advancement of pain education and research at UofT.
Such an approach also was in line with emerging concepts of the value of adopting a biopsychosocial approach to pain education, research and management. The cooperation and support of all the health sciences deans were gained, an application was put together and submitted, and this proposal was the one selected for the UofT funding.
Administrative History
The administrative HUB of the UTCSP is based in the Faculty of Dentistry, with an administrative structure and governance model that was developed over time. The 4 current active committees include the Executive, KT, Research, Education committees, as well as subcommittees, working groups and the IPC infrastructure. Dr. Michael Salter from the department of Physiology, Faculty of Medicine and Sick Children’s Hospital was the first UTCSP director (2000-2009). Dr. Bonnie Stevens from the Lawrence S Bloomberg Faculty of Nursing and Sick Children’s Hospital then became Director (2010-2019). Dr. Robert Bonin from the faculty of Pharmacy assumed the intern directorship role (2020). For the past 4, the UTCSP has been co-directed by Rob Bonin from the Faculty of Pharmacy and Rachel Bosma from the Faculty of Dentistry. Membership is from across campus across 7 different faculties and includes members from the Toronto academic hospitals.
Key Initiatives
For over 20 years, the UTCSP has delivered each year the Interfaculty Pain Curriculum to approximately 20,000 students from 78 different disciplines at UofT. These include Dentistry, Medicine, nursing, pharmacy, social work, physiotherapy, occupational therapy, physician assistants,
100 Members of the UTCSP contribute to this one-week educational initiative each year by helping to formulate each year’s programme, by giving lectures, or by acting as facilitators in break-out small-group sessions with students.
The UTCSP is also part of an educational initiative at UofT, The Pain Medicine Residency Program, which links residents with UTCSP scientists and supports pain training.
The UTCSP’s Annual Scientific Meeting brings together its members to learn more about the Centre’s recent activities and recent pain research findings from presentations by its members and invited external speakers.
Support of UTCSP trainees is provided through travel awards (e.g. to Canadian Pain Society annual meeting) and UTCSP Pain Scientist Awards, trainee orientation/welcome events, pain schools, professional development and training opportunities, and more. This has had a substantial impact; approximately 80% of UTCSP trainees remain in pain research today.
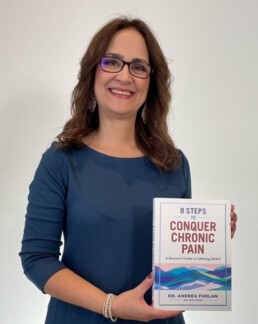
Mentor of the Month - Dr. Andrea Furlan
Introducing Dr. Andrea Furlan, a physician and Senior Scientist. Learn more about her journey, delve deeper into her extraordinary accomplishments, and uncover future prospects she envisions for the realm of pain study.
Dr. Andrea Furlan is a physician and Senior Scientist at the Kite Research Institute, Toronto Rehabilitation Institute at the University Health Network (UHN). She completed her residency in Physiatry at the University of São Paulo, Brazil and her PhD in Epidemiology at the University of Toronto, Canada. Dr. Furlan’s research largely focuses on Rehabilitation Medicine and alternative treatments for chronic pain. She has published over 100 peer-reviewed articles and has received awards such as the 2020 Pain Society of Alberta Pain Excellence Award, and the 2021 Canadian Pain Society Excellence in Pain Mentorship Award. In addition to her academic achievements, Dr. Furlan is an excellent and well-known science communicator, with a YouTube channel that teaches her 500,000 subscribers about chronic pain and its management.
We asked Dr. Furlan a few questions about her career:
What inspired you to focus on pain?
In my teen years, I suffered from terrible, debilitating, monthly menstrual cramps. I missed many social events, school days, exams, and the medications destroyed my stomach. When I got to medical school (in Brazil) I came across physiatry, the medical specialty for people with disabilities. As an intern in general internal medicine, one of the patients I admitted for investigation had pain all over her body. She ended up getting a lot better when a physiatrist came and did a single session of acupuncture. I became fascinated by the endogenous opioid system and decided to become a pain doctor, and physiatrist.
What have been some of the great highlights in your career thus far?
When I came to Canada, my first job was with the Cochrane Collaboration Back Review Group. After authoring many Cochrane reviews, I was invited to lead the research team for the first Canadian Opioid Guideline, which was published in 2010. In 2013, I heard about Project ECHO in the US. I went there with a group of colleagues from Canada, and when we returned, we started the first ECHO hub in Canada, for Chronic Pain and Opioid Stewardship, and soon we will be celebrating 10 years. We now have expanded ECHO to more than 30 conditions in Ontario, and the ECHO chronic pain has expanded to many other Canadian Provinces. More recently, I decided to start a YouTube channel, and write a book. My channel has just passed 550K subscribers and 45 million views.
What do you think is the next big thing (therapy, discovery, field of study) for pain?
I have no doubt that the next big thing will be how we tap into the brain to change neuroplasticity of pain. Every time I open a pain journal there are so many new discoveries of the amazing ability of the brain and its connections to the immune system, neuroendocrine system, and gut microbiome. I can’t keep up with all the neuroscience publications, but I think we will have a revolution in the way we treat pain, especially chronic pain.
Non-pharmacological Skill-Based Invention as an Alternative to Reduce Opioid Use in Chronic Pain
Opioids are often used to treat non-malignant pain. However, it has been suggested that opioids are not any more effective than non-opioid treatments and could potentially be harmful in the short- and long-term.
Written by:
Vaidhehi Veena Sanmugananthan
Edited by:
Georgia Hadjis
Despite this, opioids remain heavily prescribed, with over 142 million opioid prescriptions being administered in the US in 2020. The best methods to reduce opioid use are not yet clear. For example, opioid tapering has been shown to be too abrupt and lacks alternatives, which could potentially lead to harmful and suicidal behaviors. Alternatively, UTCSP scientist Dr. Andrea Furlan and her team suggest that multimodal non-pharmacological treatment approaches to improving chronic non-malignant pain may help reduce the harm associated with tapering. As such, they conducted the I-WOTCH (Improving the Wellbeing of People With Opioid Treated Chronic Pain) randomized clinical trial (RCT) to test the effectiveness of these self-management approaches to improve pain-related disability and reduce opioid use in those with non-malignant chronic pain.
Six-hundred-and-eight adult participants taking strong opioids for their non-malignant chronic pain (e.g.buprenorphine, morphine, fentanyl, methadone, oxycodone, tapentadol, tramadol, and others), were randomized 1:1 to either usual care or 3-day-long group sessions which focused on skill-based learning. Individuals who underwent the group sessions also received supplementary 1-on-1 support sessions from a nurse or lay-individual lasting 12 months. These studies were conducted in primary-care facilities in England. The primary outcome measures were the proportion of individuals that came off opioids after 12 months, and changes in the Patient-Reported Outcomes Measurement Information System Pain Interference Short Form 8a (PROMIS-PI-SF-8), which measured pain interference towards daily living.
At the 12-month follow-up, in which 433 participants returned, there were no statistically significant differences on PROMIS scores between the two groups ( −4.1 in the intervention and −3.17 in the usual care groups; between-group difference: mean difference, −0.52 [95% CI, −1.94 to 0.89]; P = .15). Discontinuation of opioids occurred in 29% (65/225) of the intervention group and 7% (15/208) of the usual care group. While serious adverse events were reported in 8% (25/305) of the intervention group and 5% (16/303) of the usual care group, none were related to the intervention itself. Four individuals received care for probable opioid withdrawal.
The results suggest that a skill-based learning intervention helped reduce patient-reported use of opioids in comparison to usual care. However, this non-pharmacological intervention did not significantly impact pain interference on daily living. The utility of these skill-based interventions as a way to reduce opioid use for chronic pain and avoid harmful effects of opioid tapering should be investigated further.
The results suggest that a skill-based learning intervention helped reduce patient-reported use of opioids in comparison to usual care.
Assessing the potential use of chairside ultrasonography in diagnosing masticatory myofascial pain syndrome
Masticatory myofascial pain syndrome is characterized by localized musculoskeletal pain in orofacial muscles such as the masseter and temporalis. In this pain syndrome, hyper-irritated nodules referred to as myofascial trigger points (MTrPs) cause local pain and mimic odontogenic pain when palpated.
Written by:
Quinn Pauli
Edited by:
Georgia Hadjis
MTrPs palpation is currently used to diagnose masticatory myofascial pain syndrome, where force is applied to masseter and temporalis muscles to assess pain and variation in muscle texture. However this examination has limited diagnostic accuracy and cannot provide information on the attributes of MTrPs. Ultrasonography, a sound wave-based imaging tool currently used in the diagnosis of musculoskeletal pathology, may have additional utility in diagnosing masticatory pain syndrome. UTCSP members Drs. Michael Goldberg, Howard Tenenbaum, Amir Azarpazhooh and their colleagues conducted a pragmatic cross-sectional clinical diagnosis study to assess the potential utility of ultrasonography in identifying MTrPs.
The primary aim of this study was to identify the concordance between ultrasonography and palpation in detecting MTrPs. Fifty-seven participants suspected of having temporomandibular disorder received both clinical palpation from a pain specialist and ultrasonography administered by a dentist. The two diagnostic methods were then compared across number of MTrPs identified, their distribution across muscle sections, and pain occurrence. The authors found that palpation identified more MTrPs and affected areas compared to ultrasonography. Ultrasonography and palpation concurred moderately-to-substantially in identifying the quantity of MTrPs and involved muscle sections, however they disagreed on the location of the MTrPs within muscle sections.
The results of this study indicate that ultrasonography, which is objective and straightforward to implement by endodontists, has the potential to be used as a diagnostic tool for masticatory myofascial pain syndrome. Compared to palpation, ultrasonography may enhance patient experience during examination while preventing misdiagnosis and unnecessary treatments that could exacerbate pain.
The results of this study indicate that ultrasonography, which is objective and straightforward to implement by endodontists, has the potential to be used as a diagnostic tool for masticatory myofascial pain syndrome.
UTCSP Translational Seminar Series with Dr. Tasha Stanton
Dr. Tasha Stanton, Associate Professor in Clinical Pain Neuroscience, from University of South Australia, speaks about ddvances in exercise-based virtual and mediated reality for chronic pain.
On Thursday May 4th 2023 from 4-6 pm, don’t miss the chance to hear from Dr. Tasha Stanton (Associate Professor in Clinical Pain Neuroscience, from University of South Australia). Dr. Stanton’s talk: Advances in exercise-based virtual and mediated reality for chronic pain. After the 45-minute talk, there will be a 15-minute Q&A, followed by light refreshments.
Hosted by the UTCSP Knowledge Translation Committee Trainee Members, this first talk in a series of translational seminars is an opportunity to hear from speakers addressing various topics related to pain-science and pain-research.
Speaker:
Dr. Tasha Stanton
Associate Professor in Clinical Pain Neuroscience, University of South Australia

Date:
Thursday, May 4th 2023
Location:
Health Sciences Building
Room 610