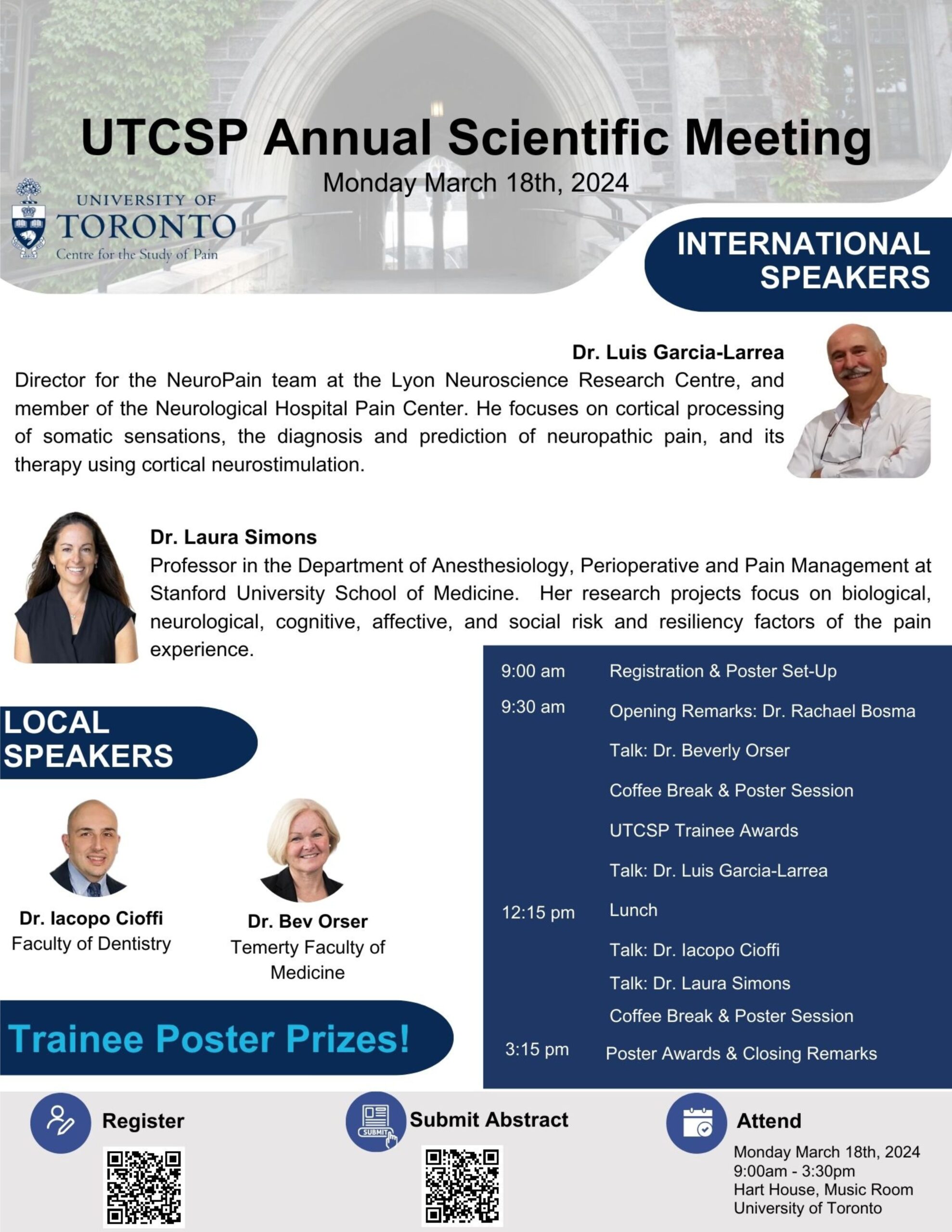
UTCSP Annual Scientific Meeting: March 18th, 2024
The UTCSP Annual Scientific Meeting is coming up soon, register today!
REGISTER HERE
SUBMIT YOUR ABSTRACT FOR THE POSTER COMPETITION HERE
We look forward to seeing you there!
UTCSP Committee Members Develop Latest Issue of Canadian Journal of Pain
Big News!
Our Knowledge Translation Committee Co-Chairs, Mariana Bueno and Hance Clarke were integral to the development of the latest issue of the Canadian Journal of Pain, highlighting trainee contributions to the field of pain. You can read their editorial, entitled: The Future Is Bright: Highlighting Trainee Contributions to the Canadian Journal of Pain here.
Some papers that involved U of T trainees/researchers include:
- Unacknowledged Pain and Disenfranchised Grief: A Narrative Analysis of Physical and Emotional Pain in Complex MAiD Bereavement Stories https://doi.org/10.1080/24740527.2023.2231046
-
The impact of preoperative patient education on postoperative pain, opioid use, and psychological outcomes: A narrative review
-
Signs and symptoms of pediatric complex regional pain syndrome - type 1: A retrospective cohort study
- Post Viral Pain, Fatigue, and Sleep Disturbance Syndromes: Current knowledge and Future Directions
https://www.tandfonline.com/doi/full/10.1080/24740527.2023.2272999?src=exp-la -
“We survived the pandemic together”: The impact of the COVID-19 pandemic on Canadian families living with chronic pain
-
The impact of preoperative patient education on postoperative pain, opioid use, and psychological outcomes: A narrative review

Join us for a CPIN-UTCSP lecture by Dr. Howard Fields
Join us for this in-person lecture by Dr. Howard Fields.
Speaker Details | Click Here

INVESTIGATING THE ROLE OF ASTROCYTE-NEURONAL METABOLIC COUPLING IN THE DEVELOPMENT OF CHRONIC PAIN - DR. GIANNINA DESCALZI
Dr. Giannina Descalzi is an Assistant Professor in the Department of Biomedical Sciences, at the Ontario Veterinary College, in the University of Guelph. Their research focuses on the intersection of pain and emotion, investigating the molecular mechanisms involved in chronic pain development and mental health disorders. Dr. Descalzi’s methods bridge animal models of chronic pain with molecular biology and systems neuroscience to enhance our understanding of chronic pain, mental health, and circuit-wide gene function. Dr. Descalzi holds a doctorate in Neuroscience from the University of Toronto, and completed a Banting postdoctoral fellowship at the Icahn School of Medicine at Mount Sinai in New York, and a second postdoctoral fellowship at NYU. Dr. Descalzi’s work is has been funded through NARSAD Young Investigator Grants, the Canadian Institutes of Health Research, the National Sciences and Engineering Research Council, the Azrieli Foundation, and the Canadian Pain Society’s Early Career Investigator Pain Research Grant.
Check Out This Podcast Episode With Dr. Patcharaporn (Nok) Srisaikaew!
UHN Trainee Podcast: Seeds of Science
From Brain Specimens to Pain Neuroimaging: A conversation with Dr. Patcharaporn Srisaikaew
In this episode, Dr. Emily Mills chats with Dr. Patcharaporn (Nok) Srisaikaew, a post-doctoral researcher in Dr. Mojgan Hodaie’s lab at the Krembil Brain Institute.
Nok completed her PhD specializing in human body dissections and the use of MRI to search for biomarkers of mild cognitive impairment. Nok’s post-doctoral research at UHN aims to elucidate the underlying neural mechanisms of limbic system (involving cognitive, memory and emotional systems) alterations in individuals with trigeminal neuralgia, a distressing facial pain condition.
Tune in to hear how she used her research expertise to help her own father who showed early signs of mild cognitive impairment.
UHN Trainee Podcast: Seeds of Science is proudly supported by the UHN Office of Research Trainees. For more information on the podcast and interviewees, visit our webpage: https://uhntrainees.ca/trainee/seeds-of-science-podcast/
LISTEN BELOW!

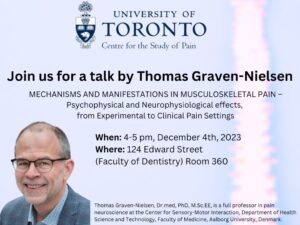
You're Invited: UTCSP Presents an In-Person Talk: Thomas Graven-Nielsen
You are invited to join us for a talk by Thomas Graven-Nielsen titled: MECHANISMS AND MANIFESTATIONS IN MUSCULOSKELETAL PAIN –Psychophysical and Neurophysiological effects, from Experimental to Clinical Pain Settings.
When: 4-5 pm, December 4th, 2023
Where: 124 Edward Street (Faculty of Dentistry) Room 360
Pre-registration not required. We look forward to seeing you there.
PAIN talks
The Quebec Network of Junior Pain Investigators (QNJPI) is proud to organize the 8th edition of the PAINtalks, which will take place at the Zoo de Granby on November 2nd, 2023 at 18:30 p.m.
Le PAINtalks is an evening of popular conferences on the theme of pain. It is a bilingual initiative, free and open to all, which is inspired by the “TED” presentation formula. Speakers are invited to submit their candidacy to present at the evening in order to communicate their research.
The team behind PAINtalks brings together students in the field of radiation sciences and biomedical imaging, experimental surgery, rehabilitation sciences, virtual rehabilitation, health sciences and psychology.
More than 800 people signed up for the PAINtalks 2022 from all over Quebec, several other Canadian provinces, as well as other countries around the world. A simultaneous translation service was offered to everyone attending the event, in person or online. All the presentations were filmed in high definition, then made available to Internet users with English and French subtitles via our website, our YouTube channel, our Twitter account and our Facebook page.
Like last year, the PAINtalks has once again partnered with three influential networks in the field of pain at the national and international levels, either with the Canadian Pain Society (CPS), la North American Pain School (NAPS) and l’European Pain School (EPS). These partnerships will, among other things, make it possible to offer a place for two of the speakers to participate in the next edition of the CPS and the NAPS.
In addition, partnerships with chronic pain networks have expanded and solidified for the 2023 edition of the PAINtalks : L’Association québécoise de douleur chronique (AQDC),Association de soutien et d’information face à la douleur (ASID), Société québécoise de fibromyalgie (SQF), Migraine Quebec, Société québécoise de la douleur (SQD), Quebec pain research network (QPRN) and l’Association des stomisés Richelieu-Yamaska.
Date:
November 2nd, 2023
18:30 p.m.
Location:
Zoo de Granby, Quebec
National Pain Awareness Week
National Pain Awareness Week is approaching!
Visit the National Pain Awareness Week Calendar to learn more and register for all the exciting events that are being hosted by various organizations and partners. Download the Calendar PDF to find links to all events listed, simply by clicking an event on the calendar.

November 6-12, 2023
Addressing the Usage of Peripheral Nerve Stimulation as a Treatment Option for Neuropathic Pain
According to the International Association for the Study of Pain, neuropathic pain (NP) is pain that arises from lesions and/or disease of the somatosensory system.
Written by:
Vaidhehi Veena Sanmugananthan
Edited by:
Georgia Hadjis
According to the International Association for the Study of Pain, neuropathic pain (NP) is pain that arises from lesions and/or disease of the somatosensory system. NP is a global health problem that is quite costly to treat. Two treatment options that have been used to treat NP are interventional pain management (IPM) and peripheral nerve stimulation (PNS). IPM includes diagnostic/therapeutic procedures administered through the skin that aim to modify pain signals in the body. Unlike other treatments of NP, like spinal cord stimulation, thus far there are no clear guidelines outlining the role and usage of PNS for NP treatment. UTCSP investigator Dr. Anuj Bhatia and colleagues surveyed international pain experts to investigate the current perception surrounding the use of IPM and PNS as treatments for NP.
A cross-sectional online survey was circulated to NP experts worldwide (pain medicine physicians, researchers, and leaders of professional pain societies). Of the 24 that responded, the most targeted areas using PNS were the distal common peroneal tibial and the sural nerves (60%). Overall, the aggregate reported NP treatment order was 1) non-opioid medications, 2) IPM which included epidural/perineural steroid injections and transcutaneous electrical nerve stimulation 3) pulse radiofrequency (RF) or RF ablation/denervation, 4) temporary PNS then permanent PNS. Half of the respondents (50%) reported that they preferred to trial non-neuromodulation treatments for 1-3 months before considering PNS. The majority of respondents (92%) believe that PNS should be administered early on in treatment plans for NP. The most common barriers reported for the use of PNS were high costs, lack of evidence supporting its usage, little to no proper training programs, and overall insufficient familiarity with the treatment.
This over-arching and broad survey is a steppingstone towards further understanding the opinions, pros and cons surrounding PNS as a treatment option for NP. However, it is clear that there still needs to be more research towards understanding PNS and the outcomes of this treatment.
This over-arching and broad survey is a steppingstone towards further understanding the opinions, pros and cons surrounding PNS as a treatment option for NP.