UTCSP Welcome October 1 at Hart House
The University of Toronto Centre for the Study of Pain is a virtual centre that brings together outstanding scientists, clinicians, educators and trainees to address the chronic pain crisis. Join us for our Welcome Event- an excellent opportunity to bring the pain community together to reconnect, meet new people, and share ideas as we kick-off this new year. The event will include a short presentation, award announcements, networking opportunities, excellent food and free drinks! All welcome! Please register here.

IASP 2024 World Congress on Pain
IASP’s World Congress on Pain is the largest gathering of pain professionals in the world, bringing together more than 5,000 scientists, clinicians, and healthcare providers from around the world and across pain disciplines. Attendees will experience a world-class lineup of more than 400 international speakers with comprehensive sessions bringing you the latest pain research and treatment.
August 5-9, 2024
Upcoming Talk by Dr. Mike Hildebrand

Summary: In this talk, Dr. Hildebrand will highlight his recent work aimed at bridging the translational divide between rodent preclinical work on spinal pain processing and new treatment approaches for humans. His team has developed new human spinal cord tissue models of pain signaling that parallel rodent in vivo and ex vivo pain models. Using these complementary approaches, they are investigating molecular mechanisms of pain processing across development, sex and species, including the regulation of excitatory glutamate receptors and neuronal excitability in dorsal horn nociceptive circuits.
Mike Hildebrand Bio: Dr. Mike Hildebrand completed his PhD in neurophysiology in Dr. Terry Snutch’s lab at UBC, followed by an industrial R&D fellowship at NeuroMed Pharmaceuticals in Vancouver. After this, Dr. Hildebrand completed an academic postdoctoral fellowship in Mike Salter’s lab at Sick Kids Hospital. Dr. Hildebrand is now leading a translational pain research program as a Professor in the Neuroscience Department at Carleton University and as an Affiliate Investigator at The Ottawa Hospital. His research team is studying mechanisms of acute and chronic pain processing using animal and human spinal cord tissue models. Dr. Hildebrand is also the Chair of the Scientific Program Committee of the Canadian Pain Society and an Associate Dean in Graduate Studies at Carleton.
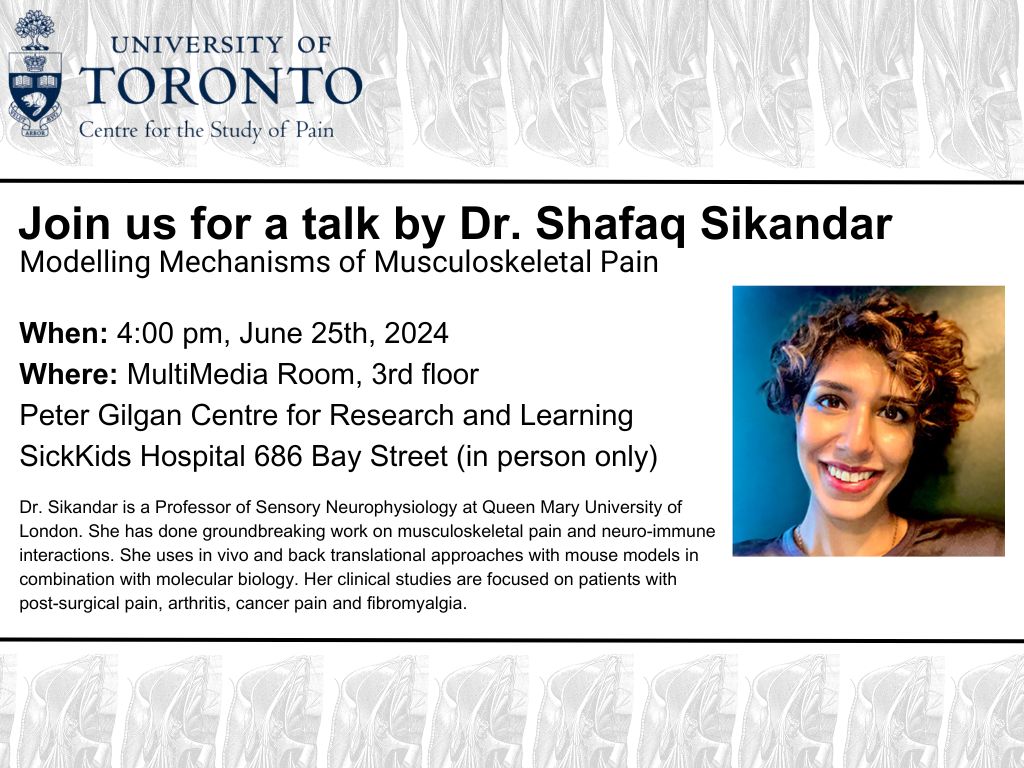
Upcoming In Person Talk by Dr. Shafaq Sikandar
The UTCSP is please to announce an upcoming in-person talk.
Dr. Shafaq Sikandar, Professor of Sensory Neurophysiology, Queen Mary University of London
Dr. Sikandar has done groundbreaking work on musculoskeletal pain and neuro-immune interactions. She uses in vivo and back translational approaches with mouse models in combination with molecular biology. Her clinical studies are focused on patients with post-surgical pain, arthritis, cancer pain and fibromyalgia.
Talk Title: ‘Modelling mechanisms of musculoskeletal pain’
June 25, 2024 4:00pm (Starts on the hour)
MultiMedia Room, 3rd floor
Peter Gilgan Centre for Research and Learning
SickKids Hospital
686 Bay Street
In person only
UTCSP EVENTS BRING TOGETHER INTERNATIONAL PAIN RESEARCHERS

UTCSP ASM and the HPSSS Highlights Featured in UofT Dentistry's Website
From March 18 to 20, 2024, the University of Toronto Centre for the Study of Pain (UTCSP) hosted two events that brought together local, national and international pain researchers. The planning for both events was overseen by Rachael Bosma, director of UTCSP and assistant professor, status only, at the Faculty, and Massieh Moayedi, chair of the UTCSP Research Committee, associate professor and Canada Research Chair (Tier 2) in Pain NeuroImaging at the Faculty.
The first event was the UTSCP Annual General Meeting, designed for the U of T pain community to showcase the scientific progress made at the university over the year, including poster presentations. It was attended by students and faculty and included four speakers: Luis Garcia-Larrea, research director for the NeuroPain team at the Lyon Neuroscience Research Centre; Laura Simons, professor in the Department of Anesthesiology, Perioperative and Pain Management at Stanford University School of Medicine; Beverly Orser, professor and chair of the Department of Anesthesiology & Pain Medicine, Temerty Faculty of Medicine; and Iacopo Cioffi, associate professor at the Faculty of Dentistry and co-director the Centre for Multimodal Sensorimotor and Pain Research (CMSPR). (read more here)
Supplementary CPIN-UTCSP lecture by Dr. Howard Fields
Join us for this supplementary virtual lecture by Dr. Howard Fields.
|
Speaker
|
Howard Fields, MD, PhD,
Professor, Neurology and Physiology Emeritus, University of California, San Francisco |
|
Title
|
The Neurobiology of Opioid Analgesia: a decisive view
|
|
Date
|
Wednesday, February 7th, 2024
|
|
Time
|
1:00 PM
|
|
Virtual Link
|
https://utoronto.zoom.us/j/88193014003
Meeting ID: 881 9301 4003, Passcode: 846011 |
|
Host
|
Derek van der Kooy, PhD,
Professor, Department of Molecular Genetics, University of Toronto |
|
Co-Sponsors
|
Department of Molecular Genetics and the University of Toronto Centre for the Study of Pain
|
Speaker Details | Click Here

Dr. Hance Clarke on CBC's The Current
Many Canadians suffer from debilitating chronic back pain, affecting their work, relationships and even mental health. We hear from researchers about a treatment called pain reprocessing therapy, which could offer some sweet relief by reframing that pain in our minds.
Listen to the segment (Dr. Hance Clarke speaks at the 15:19 minute mark) here.

Reduced excitatory neurotransmission in the hippocampus after inflammation and sevoflurane anaesthesia
Title: Reduced excitatory neurotransmission in the hippocampus after inflammation and sevoflurane anaesthesia
Author: Rossi Tomin
Editor: Georgia Hadjis
Perioperative neurocognitive disorders (PNDs) are deficits in attention, memory, executive function, and delirium that are regularly encountered postoperatively in adult patients. PNDs can be short or long-term and are correlated with additional long-term detrimental effects such as early retirement and increased mortality rates. While recently developed animal models show the combination of inflammation and general anaesthesia to be potential contributing factors, the exact mechanisms by which PNDs occur are unknown. To date, no effective preventative or treatment factors for PNDs exist. UTCSP member Dr. Beverley Orser and colleagues used an animal model to investigate the effects of an inflammatory response, coupled with application of a general anaesthetic, on excitatory synaptic transmission in the hippocampus, with an emphasis on the Schaffer collateral-CA1 pathway, which is important in learning and memory.
A previously employed animal model of anaesthetic-treated inflammation found a dysregulation in excitatory/inhibitory neurotransmission in the CA1 region of the hippocampus in the form of increased tonic inhibition , but excitatory neurotransmission was not investigated directly. To examine the excitatory component of the dysregulation, the authors generated a lipopolysaccharide (LPS) and sevoflurane inflammation/anaesthesia model and used whole-cell voltage clamp recordings to observe the activity of CA1 neurons. The authors found a reduced amplitude of miniature excitatory postsynaptic currents –which occur due to presynaptic glutamate release– that may result either from a reduction in function or quantity of postsynaptic AMPA receptors or a reduction of presynaptic glutamate release.
The results of this study, published in the British Journal of Anaesthesia, indicate a disruption in the excitatory and inhibitory balance of neurotransmission in the CA1 neurons of mice. This finding further elucidates the contribution of dysregulated neurotransmission on PNDs and provides future potential therapeutic targets for the reinstatement of excitatory and inhibitory equilibrium.
Read more here:
Khodaei, S., Wang, D. S., Orser, B. A., (2023). Reduced excitatory neurotransmission in the hippocampus after inflammation and sevoflurane anaesthesia. British Journal of Anaesthesia, BJA Open, Volume 6, 2023, 100143, ISSN 2772-6096, https://doi.org/10.1016/j.bjao.2023.100143
PASSERELLE launches the POR-Mitacs Fellowship Program
Exciting news!
PASSERELLE launches the POR-Mitacs Fellowship Program with Mitacs Canada.
PASSERELLE SPOR National Training Entity and Mitacs invite undergraduate, college and graduate students, postdoctoral fellows from all disciplines to participate in this new patient-oriented research (POR)-Mitacs Fellowship Program.
Deadline: February 9, 2024
Learn more here
Got questions? Email: info@passerelle-nte.ca

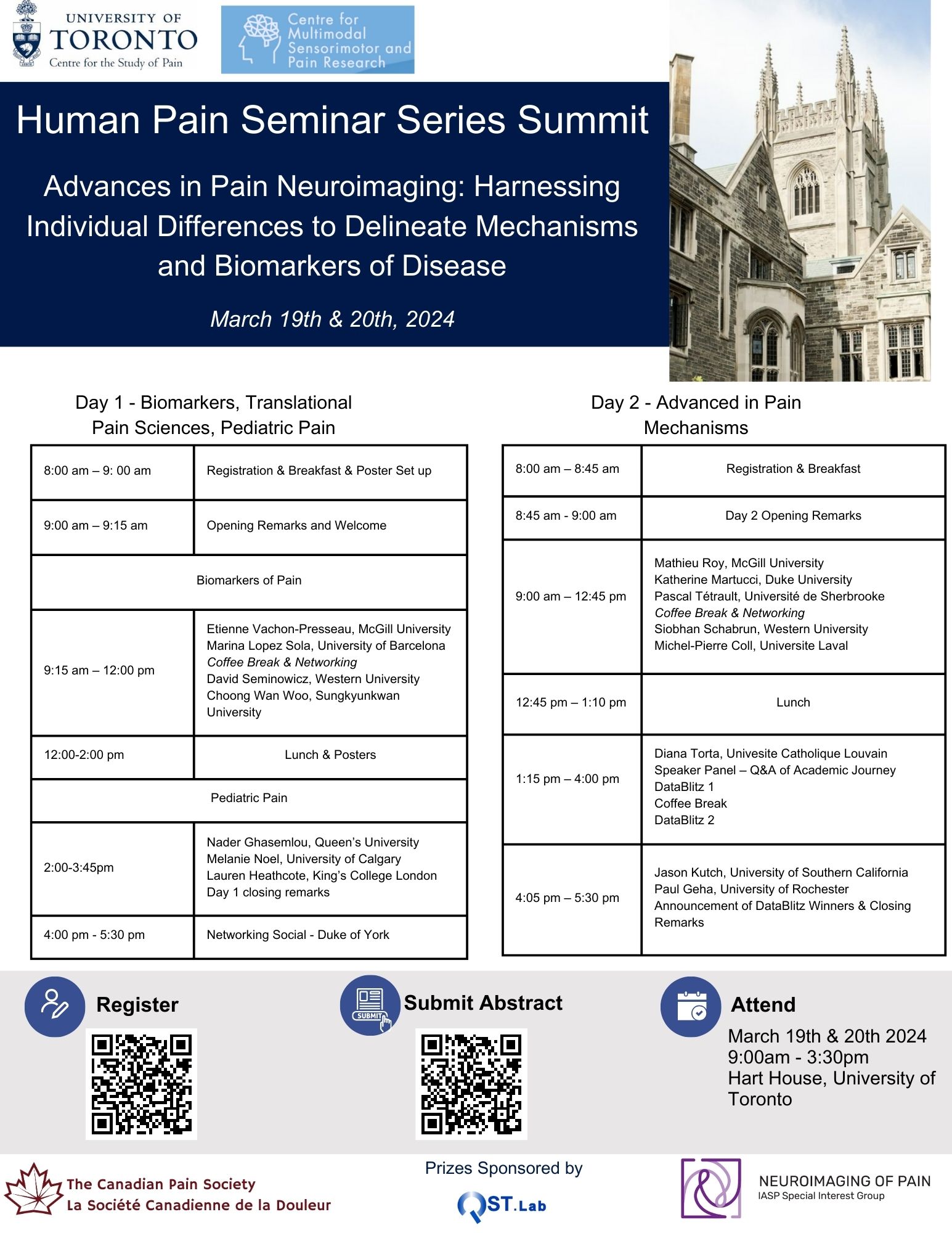
Human Pain Seminar Series Summit: March 19 & 20, 2024
The Human Pain Seminar Series Summit is coming up soon, register today!
REGISTER HERE
SUBMIT YOUR ABSTRACT FOR THE POSTER COMPETITION HERE
We look forward to seeing you there!